Extracellular vesicles
Extracellular vesicles (EV) include a wide range of lipid membrane particles secreted by all types of cells, distinctive in size, biogenesis, cargo molecules, and function. After being secreted upon the fusion of multivesicular bodies with the plasma membrane, extracellular vesicles play central roles in a variety of processes, including intercellular communication, recycling of membrane proteins and lipids, immunomodulation, senescence, angiogenesis, proliferation, differentiation, and migration. Interestingly, shed under both normal and pathological conditions, extracellular vesicles have been found in blood and other biological fluids and are considered relevant diagnostic tools and a key source in the search for novel biomarkers for disease.
On the other hand, undesired immune responses have drastically hampered outcomes after allogeneic organ transplantation and cell therapy, and also lead to inflammatory diseases and autoimmunity. Mesenchymal stem cells have powerful regenerative and immunomodulatory potential, and their secreted EV are envisaged as a promising natural source of nanoparticles to increase outcomes in organ transplantation and control inflammatory diseases. Indeed, since EVs are apparently well-tolerated, their use paves the way for innovative and more efficient cell-free therapies based in nanomedicine avoiding the putative side effects associated to stem cell transplantation.
In terms of future directions, to achieve full translation into viable therapeutic candidates from a manufacturing perspective, extravcellular vesicles processing has to further develop major issues, which include large‐scale processing in obligatory Good Manufacturing Practice conditions, quality and potency controls, and instrumentation. Accordingly, many factors in the downstream isolation, characterization, and analysis processes may have an impact on the outcome of extracellular vesicles production, but also refine their efficacy. Although the design and development of extracellular vesicles‐based products progresses toward standardized, controlled processes at the appropriate scale, the yield of extracellular vesicles is limiting. There are different cell culture or microenvironment conditions, including cell density, aging and passage, stage of differentiation, and substrate topography, which can greatly affect extracellular vesicles yield or intrinsic properties. Moreover, the use of bioreactors with high cell growth surface, media recirculation, and repeated extracellular vesicles recovery are promising for meeting clinical standards. Furthermore, implementation of routine tests of extracellular vesicles potency and optimal dose are of paramount importance. Currently, with no robust techniques for extracellular vesicles enumeration, controlling batch‐to‐batch variations is also thought‐provoking. Lastly, a huge effort has to be invested in developing precise extracellular vesicles analytical platforms to study their specific cargo and predict the potential benefits or side effects upon delivery in humans according to current regulatory restrictions. To this end, advances in purification strategies and omics‐based quantitation and analysis must be further achieved to accurately describe the molecular composition and diversity of extracellular vesicles, as well as to gain insights into understanding associated funcions.
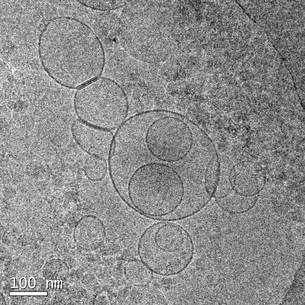
Extracellular vesicles in a peripheral blood sample from a healthy donor
Recently, the group has finished the development of a new advanced therapy product based on cardiac tissue engineering. The new product contains extracellular vesicles derived from cardiac adipose tissue mesenchymal stem cells. In specific, the novel patch, which can be adhered directly to the infarcted area by using a clinical routine surgical glue, consists of a portion of descellularised pericardial extracellular matrix filled with multifunctional nanosized extracellular vesicles (50-150 nanometers). This preliminary prototype has been successfully implanted in pigs after the induction of an acute myocardial infarction. The experiments were carried out at the Center for Comparative Medicine and Bioimaging, a research and training centre unique in Europe located on the Campus Can Ruti as well, and we analysed its benefit one-week post implantation. In particular, the aim was to study the benefit of the extracellular vesicles administration into the infarcted area in regards to the control of the host inflammatory response due its modulation could promote a reduction of the harmful postinfarction effects. Of note, an efficient release of the extracellular vesicles from the novel cardiac bioimplant to the infarcted area has been observed, as well as the formation of new blood vessels and the reduction of the pro-inflammatory cells (macrophages and T lymphocytes) infiltration within the damaged myocardium.
Monguió-Tortajada M, Prat-Vidal1 C, Martínez-Falguera D, Teis A, Soler-Botija C, Courageux Y, Munizaga-Larroudé M, Moron-Font M, Bayes-Genis A, Borràs FE, Roura S, Gálvez-Montón C. Acellular cardiac scaffolds enriched with MSC-derived extracellular vesicles limit ventricular remodelling and exert local and systemic immunomodulation in a myocardial infarction porcine model. Theranostics 2022; 12(10):4656-4670.
Soler-Botija C, Monguió-Tortajada M, Munizaga-Larroudé M, Gálvez-Montón C, Bayes-Genis A, Roura S. Mechanisms governing the therapeutic effect of mesenchymal stromal cell-derived extracellular vesicles: A scoping review of preclinical evidence. Biomed Pharmacother. 2022 Mar;147:112683.
Courageux Y, Monguió-Tortajada M, Prat-Vidal C, Bayes-Genis A, Roura S. Clinical translation of mesenchymal stromal cell extracellular vesicles: Considerations on scientific rationale and production requisites. J Cell Mol Med. 2022 Feb;26(3):937-939.
Roura S, Monguió-Tortajada M, Prat-Vidal C, Gálvez-Montón C, Bayes-Genis A. Our Journey Through Advanced Therapies to Reduce Post-Infarct Scarring. Stem Cell Rev and Rep 2021 May 22.
Monguió-Tortajada M, Prat-Vidal C, Moron-Font M, Clos-Sansalvador M, Calle A, Gastelurrutia P, Cserkoova A, Morancho A, Ramírez MA, Rosell A, Bayes-Genis A, Gálvez-Montón C, Borràs FE, Roura S. Local administration of porcine immunomodulatory, chemotactic and angiogenic extracellular vesicles using engineered cardiac scaffolds for myocardial infarction, Bioactive Materials. 2021;6:3314-3327
Monguió-Tortajada M, Bayes-Genis A, Rosell A, Roura S.. Are mesenchymal stem cells and derived extracellular vesicles valuable to halt the COVID-19 inflammatory cascade? Current evidence and future perspectives.. Thorax. 2020 Dec 15;76(2):196-200. doi: 10.1136/thoraxjnl-2020-215717
Roura S, Monguió-Tortajada M, Munizaga-Larroudé M, Clos-Sansalvador M, Franquesa M, Rosell A, Borràs FE. Potential of Extracellular Vesicle-Associated TSG-6 from Adipose Mesenchymal Stromal Cells in Traumatic Brain Injury. Int J Mol Sci. 2020 Sep 15;21(18):6761. doi: 10.3390/ijms21186761
Andrés Miguez, Sara Fernández-García, Marta Monguió-Tortajada, Georgina Bombau, Mireia Galofré, María García-Bravo, Cristina Vila, Phil Sanders, Santiago Roura, Jordi Alberch, José Carlos Segovia, Nicholas D. Allen, Francesc E. Borràs, Josep M. Canals. In vivo progressive degeneration of Huntington’s disease patient-derived neurons reveals human-specific pathological phenotypes. BioRxiv. 2020. Doi: https://doi.org/10.1101/2020.10.21.347062
Cabrera-Pérez R, Monguió-Tortajada M, Gámez-Valero A, Rojas-Márquez R, Borràs FE, Roura S, Vives J. Osteogenic commitment of Wharton's jelly mesenchymal stromal cells: mechanisms and implications for bioprocess development and clinical application. Stem Cell Res Ther. 2019 Nov 28;10(1):356. doi: 10.1186/s13287-019-1450-3
Roura S, Monguió-Tortajada M, Borràs FE. Technical challenges for extracellular vesicle research towards clinical translation. Eur Heart J. 2019 Oct 3
Monguió-Tortajada M, Gálvez-Montón C, Bayes-Genis A, Roura S, Borràs FE. Extracellular vesicle isolation methods: rising impact of size-exclusion chromatography. Cell Mol Life Sci. 2019 Mar 19
Roura S, Vives J. Extracellular vesicles: Squeezing every drop of regenerative potential of umbilical cord blood. Metabolism. 2019 Jun;95:102-104
Roura S, Bayes-Genis A. Toward Standardization of Mesenchymal Stromal Cell-Derived Extracellular Vesicles for Therapeutic Use: A Call for Action. Proteomics. 2019 Jan;19(1-2):e1800397
Roura S, Gámez-Valero A, Lupón J, Gálvez-Montón C, Borràs FE, Bayes-Genis A. Proteomic signature of circulating extracellular vesicles in dilated cardiomyopathy. Lab Invest. 2018 Oct;98(10):1291-1299
Roura S, Gálvez-Montón C, de Gonzalo-Calvo D, Valero AG, Gastelurrutia P, Revuelta-López E, Prat-Vidal C, Soler-Botija C, Llucià-Valldeperas A, Perea-Gil I, Iborra-Egea O, Borràs FE, Lupón J, Llorente-Cortés V, Bayes-Genis A. Extracellular vesicles do not contribute to higher circulating levels of soluble LRP1 in idiopathic dilated cardiomyopathy. J Cell Mol Med. 2017 Nov;21(11):3000-3009
Monguió-Tortajada M, Roura S, Gálvez-Montón C, Pujal JM, Aran G, Sanjurjo L, Franquesa M, Sarrias MR, Bayes-Genis A, Borràs FE. Nanosized UCMSC-derived extracellular vesicles but not conditioned medium exclusively inhibit the inflammatory response of stimulated T cells: implications for nanomedicine. Theranostics. 2017 Jan 1;7(2):270-284